Suppose you’ve been told to eat an anti-inflammatory diet, or maybe you’re a practitioner whose clients want to know whether this is right for them. Before hopping on this buzzy bandwagon, ask yourself ‘For what purpose?’
Without missing a beat, you say ‘Well, to reduce my inflammation!’
While technically a noble intention, let’s first acknowledge that this term is used loosely in everyday conversation, but it’s more misunderstood than one might initially believe. Let’s talk about this elephant in the room, dive in, and answer a few key questions: What’s inflammation in the first place? What factors (dietary and otherwise) contribute to, or mitigate it? And finally, how might we modify our diets and our behavior to reduce it?
What is inflammation?
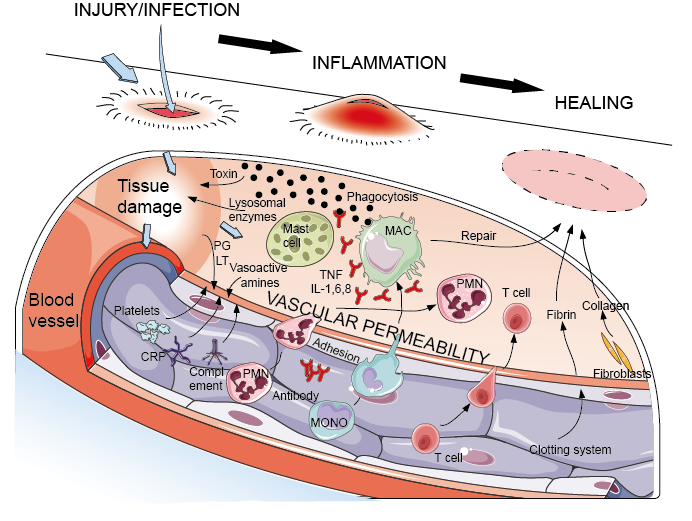
In broad terms, inflammation is the body’s immune system’s response to a stimulus.1This can be in response to common injuries such as burning your finger, or falling off of a bicycle, after which you feel the affected area become red, warm, and puffy- this is a localized response to injury, characterized by ‘increased blood flow, capillary dilation, leucocyte infiltration, and production of chemical mediators.’2In short, an inflammatory response means the innate (non-specific) immune system is ‘fighting against something that may turn out to be harmful.’
It turns out that while inflammation is often cast in a negative light, it’s actually essential in small amounts for immune-surveillance and host defense.2 In true ‘Goldilocks’ form, too little and too much inflammation both pose problems; in fact, most chronic diseases are thought to be rooted in low-grade inflammation that persists over time. This inflammation may go unnoticed by the host (you!) until overt pathologies arise, which include, but are not limited to, diabetes, cardiovascular disease, nonalcoholic fatty liver disease, obesity, autoimmune disorders, inflammatory bowel disease, and even clinical depression. This concept is called ‘The inflammation theory of disease,’ in which inflammation is the common underlying factor among the leading causes of death.3
Join ASN!
And get access to immersive learning experiences, collaboration, and networking with the greatest minds in nutrition.
How do we measure inflammation?
Although measuring low-grade chronic inflammation (read: A chronic, low-grade immune response) carries a number of limitations, studies frequently measure cellular biomarkers such as activated monocytes, cytokines, chemokines, various adhesion molecules, adiponectin, non-specific markers such as C-reactive protein, fibrinogen, and serum amyloid alpha. Key inflammatory pathways include sympathetic activity, oxidative stress, nuclear factor kappaB (NF-kB) activation, and proinflammatory cytokine production.4 Now you might wonder, ‘What does this mean for me? What modifiable factors can activate my key inflammatory pathways?’ If we are to address this question appropriately, let us turn our attention to both dietary and behavioral moderators.

What makes up an anti-inflammatory diet?
Prolonged low-grade inflammation is associated with excessive oxidative stress and altered glucose and lipid metabolism in our fat (adipose) cells, muscle, and liver.4 Therefore, research suggests that certain dietary components can modulate these key inflammatory pathways and clinical pathologies. Dr. Barry Sears explains in a review paper that “anti-inflammatory nutrition is the understanding of how individual nutrients affect the same molecular targets affected by pharmacological drugs.” 5
Compelling research from large-scale, longitudinal observational studies including the Women’s Health Initiative Observational Study6 and Multi-Ethnic Study of Atherosclerosis (MESA) study7suggest that a diet with appropriate calories that is low in refined carbohydrates, high in soluble fiber, high in mono-unsaturated fatty acids, a higher omega-3 to omega-6 ratio, and high in polyphenols, all have anti-inflammatory effects on the body. A Mediterranean diet pattern that incorporates olive oil, fish, modest lean meat consumption, and abundant fruits and vegetables, legumes, and whole grains, shows more anti-inflammatory effects when compared to a typical American dietary pattern. Other observational and interventional studies have also suggested that dietary patterns incorporating green and black tea, walnuts, ground flaxseed, and garlic are also associated with reduced inflammation.

Can my stress levels influence inflammation, too?
To conclude our discussion with anti-inflammatory dietary strategies would be a half-told story. In fact, “Communication between the systemic immune system and the central nervous system (CNS) is a critical but often overlooked component of the inflammatory response to tissue injury, disease or infection.”3
Behavioral studies have shown that prolonged psychological stress can activate the same pro-inflammatory pathways we’ve been discussing all along. While chronic psychological stress can promote over-expression of pro-inflammatory mediators, it can also promote overeating unhealthful foods in the absence of hunger. 8 Repetitively stress-eating calorie-dense, nutrient-poor foods not only further exacerbates psychological distress and creates a vicious cycle of stress-eating, but over time promotes adiposity, which we’ve described is itself a pro-inflammatory state.

Integrative strategies and considerations
This ‘cross-talk’ between the brain and body suggests that strictly dietary or strictly behavioral interventions are not enough to reduce inflammation on their own. Instead, we must consider integrative diet and lifestyle preventions/interventions simultaneously. Going forward, we’ll need better biomarkers and more research looking at individual responses to diet (personalized nutrition!), and better understanding of how food components and behavioral factors modulate genetic targets involved in the inflammatory response.
Exceptional Science & Inspiring Speakers

Get access to over 60 hours of the best science and latest clinical information at your convenience.
References:
- What is an inflammation? National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072482/. Published January 7, 2015. Accessed March 16, 2018.
- Hunter P. Stress, Food, and Inflammation: Psychoneuroimmunology and Nutrition at the Cutting Edge. EMBO Reports. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3492709/. Published November 2012. Accessed March 16, 2018.
- Hunter, Philip. The Inflammatory Theory of Disease. EMBO Reports, Nature Publishing Group, Nov. 2012, ncbi.nlm.nih.gov/pmc/articles/PMC3492709/.
- Galland, Leo. “Diet and Inflammation.” Sage, 7 Dec. 2010, journals.sagepub.com/doi/abs/10.1177/0884533610385703?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub=pubmed.
- Sears, Barry, and Camillo Ricordi. “Anti-Inflammatory Nutrition as a Pharmacological Approach to Treat Obesity.” Journal of Obesity, Hindawi Publishing Corporation, 2011, ncbi.nlm.nih.gov/pmc/articles/PMC2952901/.
- Thomson, C A, et al. “Association between Dietary Energy Density and Obesity-Associated Cancer: Results from the Women’s Health Initiative.” Journal of the Academy of Nutrition and Dietetics., U.S. National Library of Medicine, ncbi.nlm.nih.gov/pubmed/28826845.
- “Associations of Dietary Long-Chain n-3 Polyunsaturated Fatty Acids and Fish With Biomarkers of Inflammation and Endothelial Activation (from the Multi-Ethnic Study of Atherosclerosis [MESA]).” The American Journal of Cardiology, Excerpta Medica, 4 Mar. 2009, www.sciencedirect.com/science/article/pii/S0002914909001088?via=ihub.
- Tryon, M., Carter, C., DeCant, R. and Laugero, K. (2013). Chronic stress exposure may affect the brain’s response to high calorie food cues and predispose to obesogenic eating habits. Physiology & Behavior, 120, pp.233-242.




